Candida Intertrigo (Candidiasis of Large Skinfolds)
Description
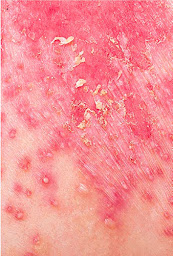
- Pink to red maceration, occurring where two skin folds come together.
- Warm moist environment leads to disruption of the skin barrier, predisposing to yeast infection.
History
- Predisposing factors include obesity, immunodeficiency (e.g. diabetes, prednisone), hot humid weather, poor hygiene, tight-fitting clothing, and use of topical steroids.
Skin Findings
- Red moist, glistening plaques with satellite pustules and papules with a fringe of white scale.
- Painful fissures frequently occur deep within the skin folds.
Laboratory
- Potassium hydroxide wet mount preparation from a pustule or scaly border shows spores and pseudohyphae.
- Skin biopsy and a surface culture may be necessary in treatment-resistant cases.
Course and Prognosis
- Candida intertrigo usually recurs if the underlying conditions are not corrected.
Differential Diagnosis
- Inverse psoriasis
- Seborrheic dermatitis
- Erythrasma
- Streptococcal infection
- Irritant contact dermatitis
Treatment
- Apply wet dressings (tap water or Burow’s solution [aluminum acetate 1 : 40 solution]) with a soft cotton cloth for 20 minutes several times per day to soothe and dry the area.
- Application of an antiyeast cream (e.g. nystatin) or an antifungal (e.g. econazole) cream should be applied twice daily in a thin layer.
- Oral antifungal agents (e.g. fluconazole 100–200 mg per day for 1 week) treat resistant or severe cases.
- Sealing in the skin with a light moisturizer (e.g. Vanicream Lite or Lubriderm) may prevent recurrences by decreasing friction and acting as a protective barrier.
- Powders may be helpful to wick away moisture but may clump if there is excessive moisture.
- Patients should be encouraged to lose weight and avoid tight-fitting clothing.
Pearls
- Nystatin is not effective for dermatophyte infections, and griseofulvin and terbinafine are not effective for yeast infections.
- Consider streptococcal infection if the rash is painful and malodorous.
- Topical corticosteroid use may predispose to yeast and dermatophyte infection.
- Patients who do not respond to antiyeast medications may have inverse psoriasis.